OPINION | Living with HIV in time of Corona

We Wear the Mask…….!!!!
We smile, but, O great Christ, our cries
To thee from tortured souls arise.
We sing, but oh the clay is vile
Beneath our feet, and long the mile;
But let the world dream otherwise,
We wear the mask ~~ Paul Laurance Dunbar
As of August 26, 2020, over 24 million people worldwide have been diagnosed with COVID-19, the disease caused by the novel coronavirus (i.e., SARS-CoV-2). Of the nearly 40 million people living with HIV (People Living with HIV - PLHIV) worldwide, most live in countries with poor healthcare infrastructure and the majority are over age 50 in several countries. Advanced age and coexisting chronic diseases are associated with severe manifestations and higher mortality from COVID-19, putting many PLHIV at increased risk. Alarmingly, two of the three countries with the highest number of HIV infections - South Africa and India - are also among the countries with the highest COVID-19 burdens.
Journal of Virus Eradication
At the very beginning of the pandemic, I somehow thought and believed that living with HIV and taking Anti retro virals (ART) would protect me from the novel Corona Virus, but I now realised that having HIV and taking ART does not confer protection against severe manifestations of COVID-19.
Several studies looking at antiretroviral drugs against HIV to treat SARS-CoV-2 have shown no mortality benefit. Some friends have asked me whether Covid 19 is an opportunistic infection, but I can assure whoever reads this, that it is not.
Some of the most disadvantaged in the COVID-19 era are people living with HIV/AIDS, the high-risk groups (Injecting Drug Users, Sex Workers and the LGBT Community) and other autoimmune diseases.
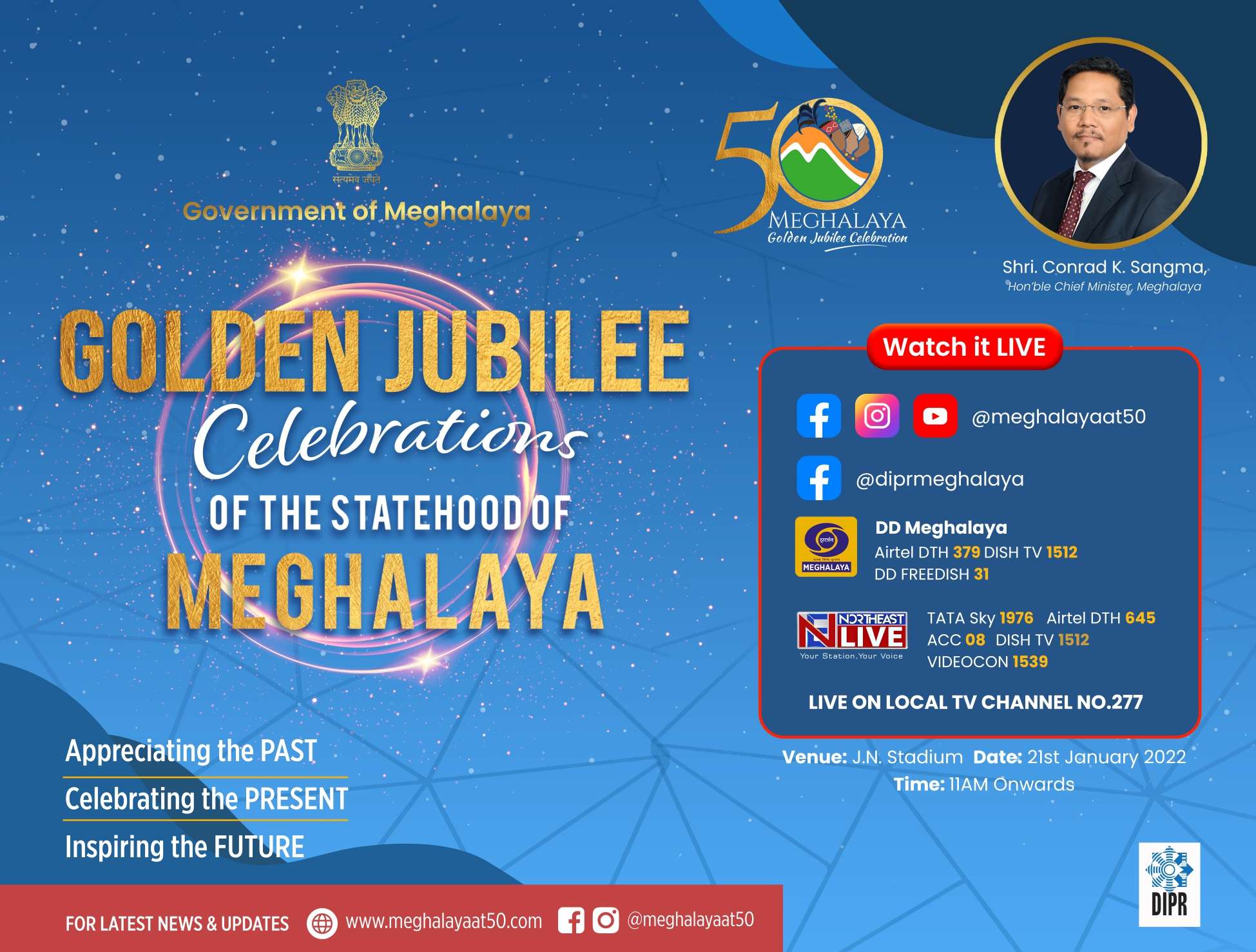
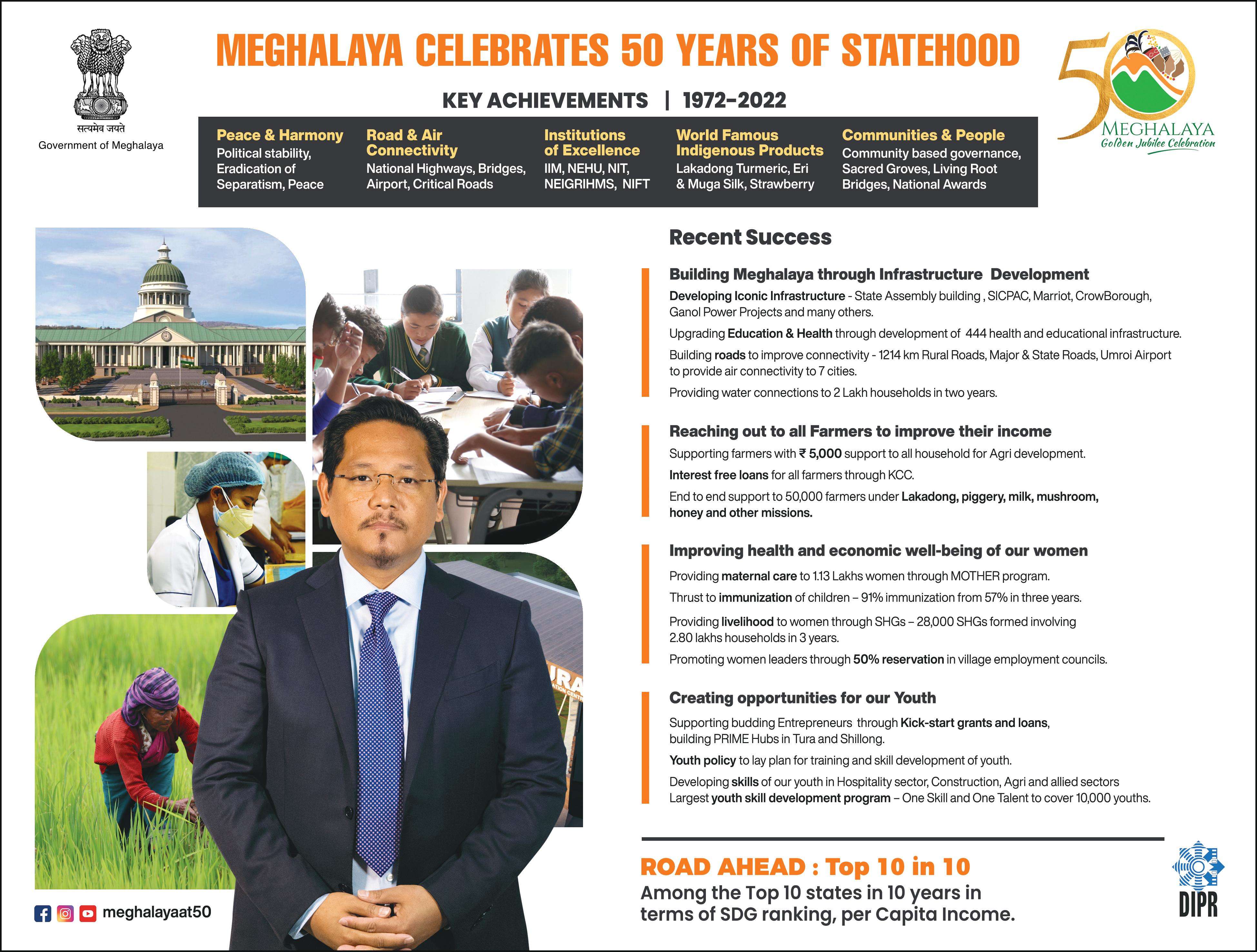
Although the number of new HIV infections has decreased globally and at the national level but in Meghalaya, the number of HIV infections is increasing, lest we forget our state has the highest Syphilis case, and many subpopulations remain at a high risk of infection due to lack of or limited access to:-
>> Lack of or limited access to Prevention services such as the Needle Syringes Exchange Program run by TI (Target Intervention) NGO, Oral Substitution Therapy as well as commodities such as condoms, etc), as well as clinical care and treatment. Lack of access to such treatment, clinical care and prevention services may lead to widespread HIV infection among the High-risk groups.
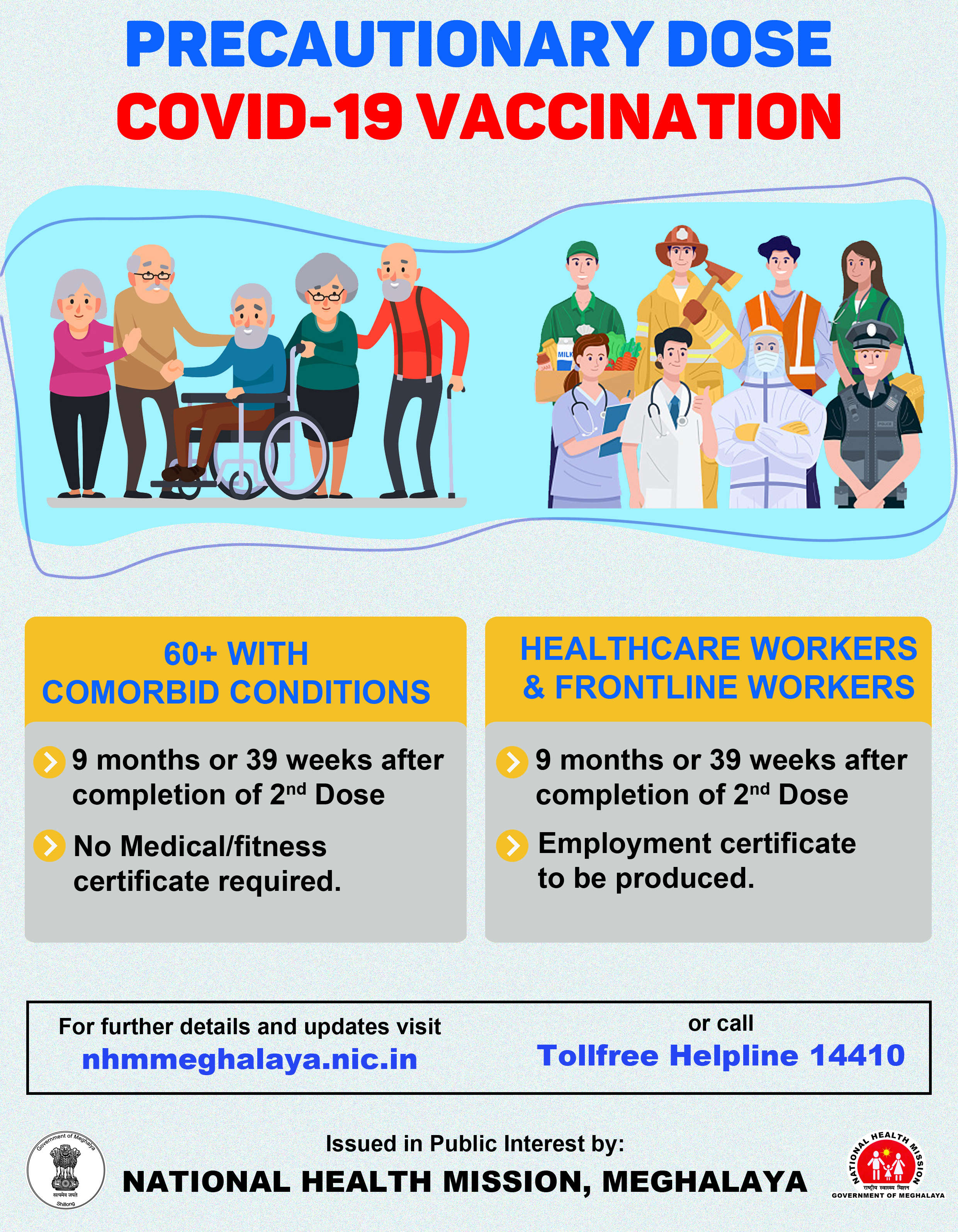
>> The pandemic has also greatly impacted PLHIV in getting their monthly refills of (Antiretrovirals) ARVs due to lockdown, exorbitant charges of transportation, no transportation and other such protocols. PLHIV, if not adhere to HIV ARVs, may develop drug resistance which may pose a problem for the entire state in the near future.
>> People Living with HIV and the High-Risk Groups are also prone to other infections like TB, Malaria, Hepatitis C and B. Research has shown that HIV/TB co-infection accelerates the damaging progression of the disease and that antiretroviral therapy (ART) initiation must be timed to increase adherence and decrease adverse effects of drug interactions. The pandemic has led to significant changes in health service delivery and amplified fears of increased death and illness.
>> The negative consequences of COVID-19 for PLHIV and the High-Risk groups are more severe than others, including job loss, food insecurity, inability to manage existing conditions, and inability to maintain preventive measures such as social distancing and use of personal protective equipment (PPE).
>> The social support and community mobilisation approaches for the management of HIV/AIDS, as opposed to individual-level approaches alone, have been shown to improve antiviral medication adherence. However, due to the enforcement of social distancing and other restrictions in the current pandemic, there has been a shift in the mechanism by which PLHIV receive such social support.
>> An additional concern for those living the HIV is the double stigma and breach of confidentiality (HIV status) that may arise if they also test positive for COVID-19. The compounded HIV/COVID-19 stigma may lead to failure to seek care.
Thus, coordinated efforts from community stakeholders, civil society, public health agencies, and healthcare providers may be essential for addressing health inequities for PLHIV resulting from social stigma and poor access to PPE, preventative services and treatment.
The important challenges for PLHIV that need to be addressed during the current pandemic are access to their antiviral refills and maintenance of their social and mental systems.
(Edited by Ibankyntiew Mawrie)
TNT-The Northeast Today is now on WhatsApp. CLICK HERE to receive more updates on your phone.
ALSO WATCH: